It's 2025, we have smartwatches that count steps and cars that drive themselves – yet most hospitals still rely on manual vitals checks every four hours and clipboards to track million-dollar equipment. The disconnect is staggering. While consumers live in an interconnected world where devices anticipate needs, healthcare facilities operate with fragmented systems that can't tell you if a ventilator needs maintenance until it fails mid-surgery. The IoT healthcare market is exploding from $89 billion to a projected $289 billion by 2028, and it's not because hospitals suddenly love gadgets – it's because IoT solves critical problems that kill patients and budgets.
IoT in healthcare extends far beyond fitness trackers and smart pills. We're talking about comprehensive ecosystems where cardiac monitors predict arrests 6 hours early, hospital beds automatically alert when high-fall-risk patients attempt to stand, and entire facilities self-optimize based on real-time patient flow. Remote patient monitoring keeps chronically ill patients at home while maintaining hospital-grade observation. Smart hospitals orchestrate thousands of connected devices to reduce errors, predict equipment failures, and ensure the right resources reach the right patients at the right time. This isn't futuristic speculation – it's operational reality transforming healthcare delivery today.
What Is IoT in Healthcare?
IoT in healthcare means connected medical devices and sensors that collect, transmit, and analyze patient data without human intervention. Unlike consumer IoT that tracks steps or adjusts thermostats, medical IoT handles life-critical data: continuous glucose readings, real-time cardiac rhythms, ventilator performance metrics, even hand hygiene compliance. These aren't standalone gadgets – they're nodes in an intelligent network that transforms raw signals into clinical insights.
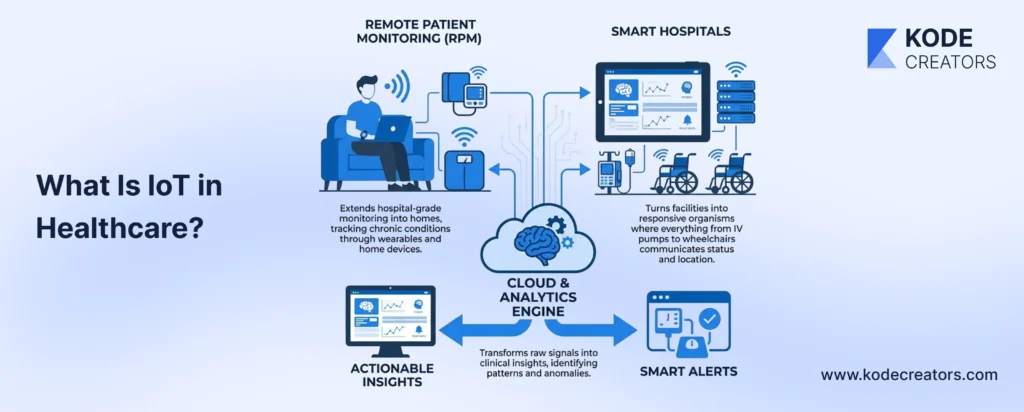
Remote Patient Monitoring (RPM) and Smart Hospitals represent two sides of the same IoT revolution. RPM extends hospital-grade monitoring into homes, tracking chronic conditions through wearables and home devices. Smart Hospitals turn facilities into responsive organisms where everything from IV pumps to wheelchairs communicates status and location. Both rely on the same fundamental architecture just deployed differently – one reaches outward to patients, the other optimizes inward operations.
The ecosystem follows a clear data path: medical devices equipped with sensors capture physiological or operational data, transmit through secure gateways that aggregate and encrypt information, push to cloud platforms for storage and processing, run through analytics engines that identify patterns and anomalies, then deliver actionable insights to clinician dashboards in real-time. Each link in this chain must be HIPAA-compliant, reliable, and fast enough for clinical decision-making. When properly implemented, clinicians see not just numbers but predictive insights that prevent complications before symptoms appear.
Remote Patient Monitoring (RPM): IoT Beyond the Clinic
Chronic Disease Management is where RPM proves its worth daily. Heart failure patients wearing connected patches generate 250,000 data points per day – impossible for humans to analyze but perfect for algorithms detecting subtle rhythm changes. One cardiology practice reduced hospitalizations by 38% after implementing continuous monitoring that caught deterioration patterns 72 hours before symptoms appeared. Diabetics using CGMs paired with insulin pumps achieve glucose control that manual monitoring never could. Blood pressure monitoring finally becomes useful when smart cuffs take readings during actual daily stress, not just relaxed doctor visits. The technology stack involves medical-grade sensors meeting FDA accuracy standards, edge processors for real-time analysis, and encrypted data streams that satisfy both clinical and compliance requirements.
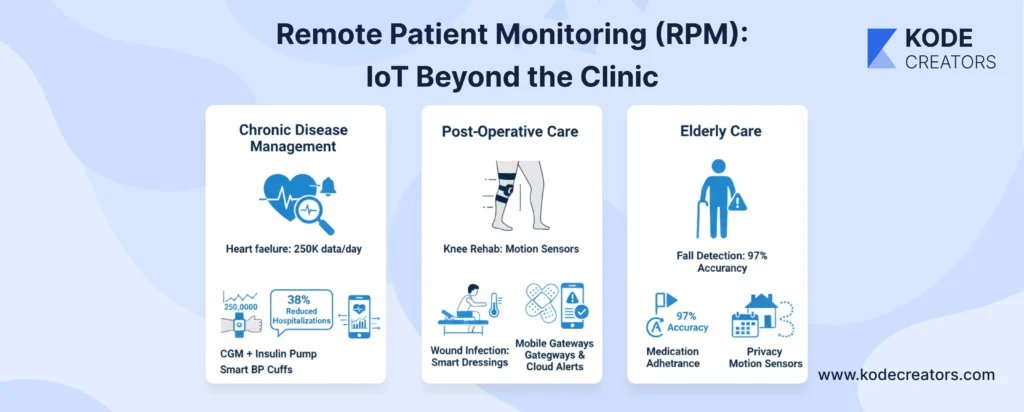
Post-Operative Care keeps patients home without sacrificing safety. After knee replacement, motion sensors track whether patients are hitting physical therapy milestones – not self-reported "feeling fine" but actual degrees of flexion achieved. Smart surgical dressings with embedded temperature sensors caught infections in trial studies 3.2 days earlier than visual inspection. The technical architecture requires careful orchestration: wearable sensors collecting data, mobile gateways aggregating streams, cloud platforms running predictive models, and APIs pushing alerts to care teams when intervention thresholds are crossed.
Elderly Care addresses the massive gap between independence and safety. Fall detection systems now combine accelerometers with barometric pressure sensors – distinguishing between sitting quickly and actual falls with 97% accuracy. Medication adherence monitoring goes beyond simple pill dispensers; smart systems track prescription refills, correlate missed doses with health changes, and adjust reminder strategies based on response patterns. Privacy-preserving motion sensors map daily routines without cameras, alerting families when Dad hasn't left the bedroom by noon or Mom's bathroom visits triple overnight.
Emergency Response happens in milliseconds, not minutes. Edge computing on devices means critical alerts don't depend on internet connectivity. When oxygen saturation crashes or cardiac arrest patterns emerge, local processors trigger immediate alerts while simultaneously streaming full telemetry to response teams. EHR integration provides instant context – responding physicians see not just "heart rate 180" but complete medication lists, recent ECGs, and relevant history.
Smart Hospitals: IoT Inside the Walls
Smart hospitals evolved from tracking individual devices to orchestrating entire ecosystems where thousands of connected components optimize themselves continuously. Asset tracking eliminates the absurd reality of nurses spending 21 minutes per shift hunting equipment. RFID tags on everything from wheelchairs to infusion pumps provide real-time location data. When code blue hits, the nearest crash cart's location appears instantly on responder screens. One hospital recovered $3 million in "lost" equipment simply by implementing IoT tracking – devices weren't missing, just hoarded in departments.
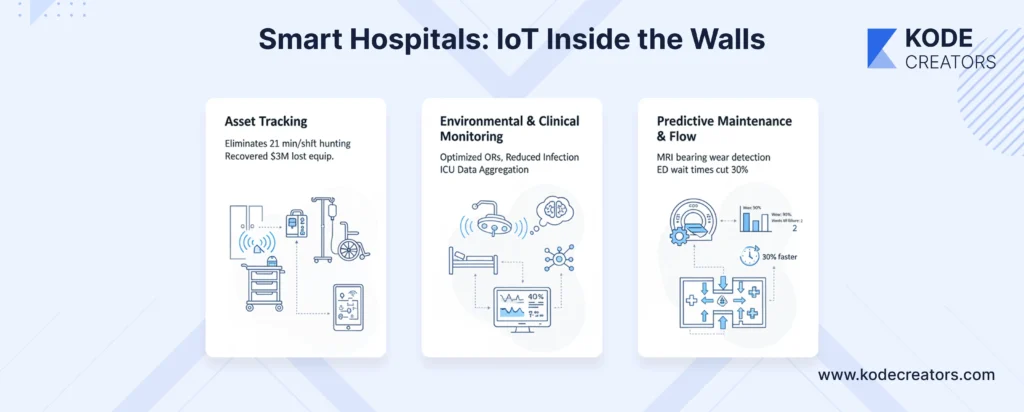
Environmental monitoring goes beyond comfort to clinical outcomes. IoT sensors adjust OR temperature and humidity for optimal surgical conditions, reduce infection rates through air quality management, and dim lights automatically for patient circadian rhythms. Connected ICUs aggregate data from 12-15 devices per bed into unified displays. Instead of checking multiple monitors, clinicians see integrated views where ventilator settings, cardiac rhythms, and lab results converge into actionable intelligence. Smart operating rooms record everything – who touched what instrument when, temperature fluctuations during procedures, equipment usage patterns that predict optimal replacement cycles.
Predictive maintenance transforms from reactive scrambling to proactive scheduling. Vibration sensors on MRI machines detect bearing wear weeks before failure. Temperature monitoring in refrigeration units prevents vaccine spoilage. IoT-enabled imaging equipment schedules its own maintenance based on usage patterns and performance degradation. Patient flow optimization uses occupancy sensors, admission predictions, and discharge planning algorithms to move patients through facilities efficiently. Emergency departments reduce wait times by 30% when IoT systems predict surge patterns and automatically adjust staffing alerts.
Key Benefits of IoT-Driven Healthcare Systems
Clinical Efficiency changes the entire diagnostic game. Instead of waiting for scheduled labs to reveal kidney function decline, continuous monitoring catches creatinine trends while intervention still matters. Emergency physicians no longer guess about the last four hours – they see exactly when chest pain started, how vitals progressed, what triggered the event. One cardiac unit cut diagnosis time in half simply because IoT devices captured the actual arrhythmia instead of relying on patient descriptions of "feeling funny."
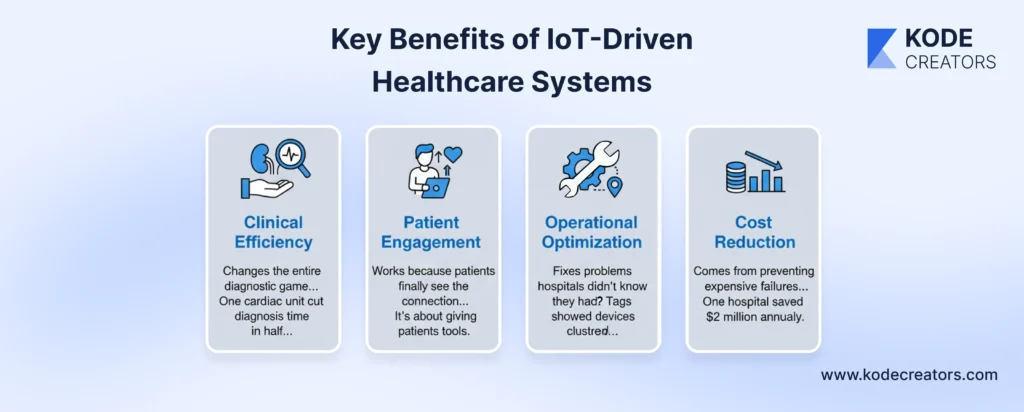
Patient Engagement works because patients finally see the connection between actions and outcomes. That diabetic who swears they follow their diet can't argue with glucose spikes after "just one cookie." Heart patients understand medication importance when they watch their blood pressure normalize in real-time. It's not about surveillance – it's about giving patients tools to actually participate in their care rather than being passive recipients.
Operational Optimization fixes problems hospitals didn't know they had. That MRI machine that always seems broken on Mondays? IoT sensors revealed weekend shutdown procedures were causing thermal stress. The mysterious equipment shortage? Tags showed devices clustered in specific departments like hoarded treasure.
Cost Reduction comes from preventing expensive failures, not cutting services. One hospital saved $2 million annually just from preventing refrigeration failures that spoiled medications. Readmission penalties disappear when problems get caught at home instead of returning as emergencies.
Data-driven decisions mean protocols based on evidence, not tradition. When analytics show certain post-op patients safely discharged two days earlier with RPM, that's millions saved without compromising care.
Data Security and Compliance
Medical IoT security isn't optional – it's existential. Every connected insulin pump, cardiac monitor, and smart bed becomes a potential attack vector. Encryption starts at the sensor level: TLS 1.3 for all transmissions, AES-256 for stored data, including temporary device caches most people forget exist. That innocent-looking temperature sensor? If it connects to the network, it needs military-grade encryption because hackers don't discriminate between device types when hunting for network entry points.
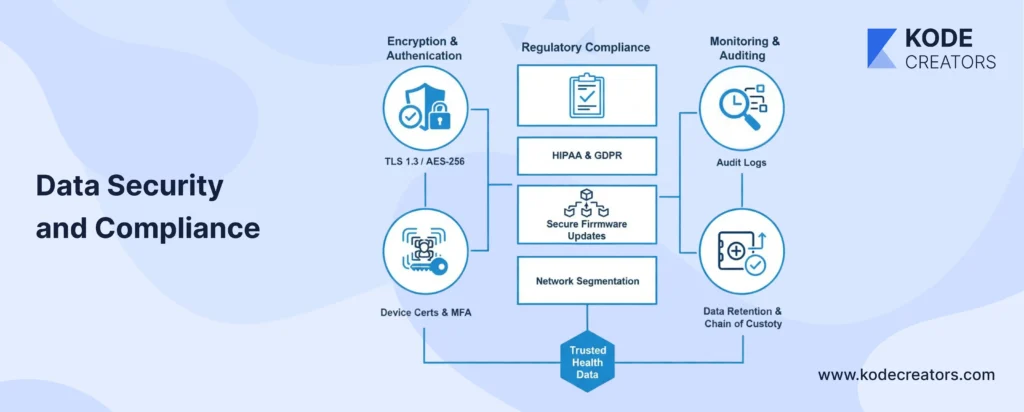
Authentication in IoT frameworks requires multiple layers. Device certificates ensure only authorized equipment joins networks. Role-based access controls determine who sees what data streams. Multi-factor authentication protects administrative interfaces. But here's what kills implementations: default passwords on medical devices. One hospital discovered 400 devices still using "admin/admin" credentials – each one a welcome mat for ransomware.
HIPAA compliance extends to every IoT component manufacturer, not just hospitals. That sensor vendor, gateway provider, cloud platform – all need Business Associate Agreements and matching security standards. GDPR adds complexity for any system touching EU patient data. Firmware updates can't be afterthoughts; medical IoT devices need secure update mechanisms that don't disrupt clinical operations. Network segmentation isolates IoT devices from critical systems – when a smart thermostat gets compromised, it shouldn't reach patient records.
Audit logs must capture everything: device connections, data access, configuration changes, failed authentication attempts. These logs become evidence during breach investigations and compliance audits. Storage and retention policies for IoT telemetry data need careful planning – it's not just about keeping records, but proving chain of custody for data that might influence clinical decisions.
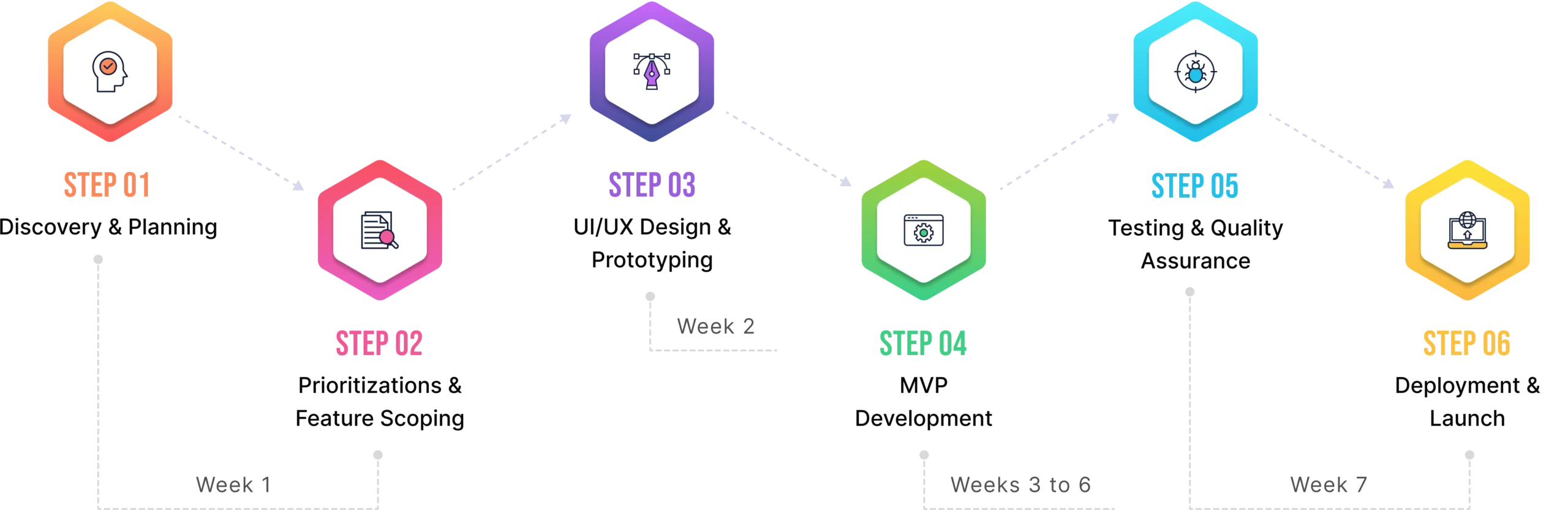
Implementation Roadmap: From Pilot to Smart Hospital Infrastructure
Step 1: Assessment starts with problems, not technology. Which department hemorrhages money on readmissions? Where do nurses waste hours hunting equipment? RPM for heart failure patients might save millions, while asset tracking solves immediate operational chaos. Define measurable goals – "reduce readmissions 25%" beats "improve patient care."
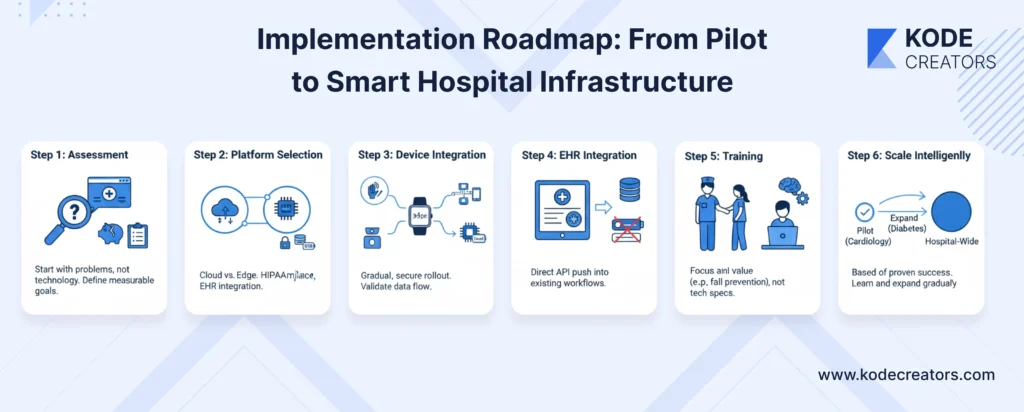
Step 2: Platform Selection determines everything downstream. Cloud-native platforms scale better but require robust internet. Edge computing handles network outages but needs on-site expertise. Choose platforms with healthcare-specific features: built-in HIPAA compliance, medical device certifications, proven EHR integrations.
Step 3: Device Integration happens gradually. Start with one device type, establish secure gateways, validate data flow. Don't connect 500 devices day one – that's how security disasters happen.
Step 4: EHR Integration makes or breaks clinical adoption. If IoT data requires separate logins, clinicians won't use it. APIs must push data directly into existing workflows.
Step 5: Training focuses on value, not features. Show nurses how IoT alerts prevent patient falls, not how MQTT protocols work. Technical staff need deeper training on troubleshooting and security.
Step 6: Scale Intelligently based on proven success. That successful cardiology RPM pilot? Expand to diabetes before tackling hospital-wide deployment. Each expansion teaches lessons that prevent costly mistakes.
Future Trends: IoT 2.0 in Healthcare (2025 and Beyond)
Edge AI puts intelligence directly on devices, analyzing cardiac rhythms on the monitor itself rather than streaming to clouds. This means predictions in milliseconds, functioning during network outages, and reduced bandwidth costs. Ventilators will adjust settings autonomously based on real-time lung compliance patterns.
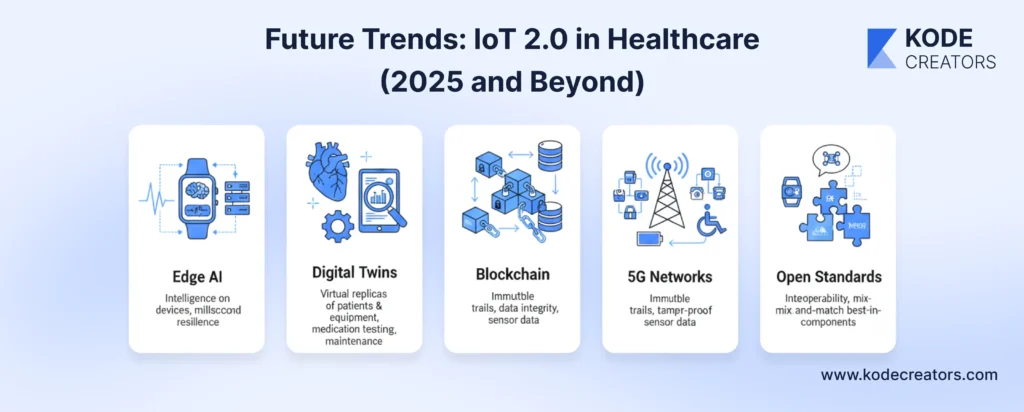
Digital Twins create virtual replicas of patients and equipment. Your digital heart, built from years of IoT data, lets doctors test medications virtually before prescribing. MRI digital twins predict component failures by simulating wear patterns under actual usage conditions.
Blockchain solves IoT's trust problem. When twenty devices contribute to a diagnosis, blockchain provides immutable audit trails proving data integrity. No more questioning whether sensor data was tampered with during transmission.
5G Networks enable massive IoT deployments previously impossible. Thousands of devices per hospital floor, streaming high-resolution data without lag. Low-power wide-area networks mean sensors running for years on coin batteries, monitoring everything from wheelchair locations to refrigerator temperatures.
Open Standards finally break vendor lock-in. The emerging Internet of Medical Things (IoMT) standards mean devices from different manufacturers actually work together. Hospitals won't need single-vendor ecosystems – they'll mix best-in-class components that speak the same language.
Conclusion:
The gap between connected hospitals and traditional facilities widens every day. One cardiac unit prevents 40% of readmissions through continuous monitoring while another still relies on patients remembering to check blood pressure. One OR predicts equipment failures weeks in advance while another scrambles when ventilators die mid-surgery. The technology transforming these outcomes exists today – proven, affordable, and ready to deploy. Healthcare organizations face a clear choice: build comprehensive IoT infrastructure that turns facilities into intelligent, responsive care systems, or watch competitors deliver better outcomes at lower costs while you manage preventable crises. Patients already track everything from sleep to steps on personal devices. They won't accept hospitals that can't match their smartwatch's sophistication much longer.