Your smartwatch can detect irregular heartbeats a week before you feel anything wrong. A fitness band can notice subtle sleep pattern changes that predict burnout before you crash. This isn't science fiction – it's happening right now in millions of wrists worldwide. The global wearable medical device market is racing toward $195 billion by 2027, driven not by fitness enthusiasts counting steps but by healthcare systems realizing that continuous monitoring prevents disasters cheaply than treating them.
Wearables have evolved from glorified pedometers to sophisticated medical instruments that rival hospital equipment. Today's devices detect atrial fibrillation with 98% accuracy, track glucose without needle sticks, and identify respiratory infections days before symptoms appear. Modern wearables combined with AI don't just tell you what's happening; they forecast what's coming. Healthcare is shifting from reactive treatment to proactive prevention, and wearables are the infrastructure making it possible. Let’s learn more about the future of wearable tech in preventive healthcare in this blog.
The Evolution of Wearable Healthcare Technology
The first fitness trackers were basically expensive pedometers that gamified walking. Remember celebrating 10,000 steps while having no idea what that number actually meant for your health? Early heart-rate monitors required uncomfortable chest straps and gave readings so inconsistent that serious athletes ignored them. These devices generated data that nobody knew how to use – pages of numbers that meant nothing to doctors and confused users. The quantified self movement was more about collecting than understanding, producing beautiful graphs of useless information.

The pandemic changed everything. Suddenly, blood oxygen levels mattered to everyone, not just mountaineers. The 2020-2024 period witnessed wearables transforming into legitimate medical devices. Apple Watch Series 4's FDA-cleared ECG capability marked the turning point – consumer devices performing hospital-grade diagnostics. Continuous glucose monitors escaped the diabetes-only category, helping anyone understand their metabolic health. Temperature tracking evolved from basic fever detection to predicting illness onset through subtle baseline variations. SpO2 sensors that once cost thousands became standard in $200 fitness bands. More importantly, the data became actionable – irregular heart rhythm notifications sent people to cardiologists, discovering undiagnosed atrial fibrillation in thousands who felt perfectly fine.
The 2025 horizon brings convergence that changes the game entirely. AI algorithms now process continuous data streams from multiple sensors, identifying patterns impossible for humans to spot. Biosensing fabrics turn clothing into medical monitors – shirts tracking respiratory rate through chest expansion, socks detecting diabetic foot problems before they become amputations. Edge computing means your watch doesn't just collect data; it runs complex predictive models locally, alerting you to health risks while maintaining privacy. We've moved from counting steps to predicting strokes, from tracking sleep to preventing mental health crises. The ecosystem finally delivers what early wearables promised: not just numbers, but knowledge that changes outcomes. Healthcare providers now treat wearable data as seriously as lab results, integrating continuous monitoring into standard care protocols.
Preventive Healthcare Reimagined Through Wearables
Wearables have shifted healthcare from treating disease to preventing it entirely, using continuous monitoring to catch problems months or years before traditional medicine would notice. The technology transforms every moment into a health assessment, turning daily life into preventive care without requiring conscious effort from users.

Early Detection runs 24/7 while you sleep, work, and forget you're wearing anything. Cardiac algorithms process every single heartbeat – not the 30-second snapshot your doctor gets annually – finding dangerous patterns in the noise of normal life. Glucose monitors catch the slow creep toward diabetes that fasting tests miss because they see what happens after meals, during stress, at 3 AM. Sleep apnea, which most people blame on getting older or being tired, gets flagged when breathing patterns show dozens of micro-interruptions nobody feels. The newest research shows wearables picking up fever patterns before you feel sick – your body starts fighting infections long before you reach for Tylenol.
Lifestyle Management finally works because it stops pretending everyone's the same. Your wearable figures out you hate morning workouts but will walk after dinner. It learns your stress eating happens at 3 PM, not randomly, and suggests alternatives before you raid the vending machine. Sleep advice isn't generic "get eight hours" nonsense – it identifies why you wake at 2 AM and what actually helps you specifically, not some study group in Finland.
Chronic Disease Prevention catches the slow-motion disasters that kill most people. Blood pressure creeping from 120 to 130 to 140 over a decade gets intercepted at 125. Weight gain that "suddenly" appears at 50 actually started at 35 – wearables document the pound-per-year trajectory everyone ignores until clothes don't fit.
Population Health departments finally work with reality instead of wishful thinking. Wearable data shows actual activity levels, real sleep patterns, true stress indicators – not the lies people tell on surveys about exercising "regularly" and eating "pretty healthy."
Key Technologies Powering the Next Generation of Wearables
Advanced Sensors are breaking through skin barriers without breaking skin. Non-invasive glucose monitoring through optical sensors and micro-needles shorter than nerve endings means diabetics ditch finger pricks. Hormone tracking via sweat analysis catches cortisol spikes and fertility windows. Hydration sensors prevent the dehydration that sends thousands to ERs – they measure electrolyte balance, not just remind you to drink water. These aren't incremental improvements; they're accessing biomarkers previously requiring blood draws.

AI & Machine Learning transform noise into knowledge. Raw sensor data means nothing until algorithms identify the pattern suggesting tomorrow's migraine or next week's depression episode. The processing happens locally now – your watch running neural networks that previously required server farms. Predictive models trained on millions of users spot your personal danger signals, not population averages.
IoT Connectivity makes wearables part of larger health ecosystems. Your watch talks to your smart scale, thermostat, and medication dispenser, creating comprehensive health pictures. EHR integration means doctors see continuous data, not snapshot vitals during visits. The connectivity works both ways – clinical updates adjust wearable monitoring parameters automatically.
Edge Computing keeps processing on your wrist, not in the clouds. Privacy improves, battery life extends, and alerts fire instantly without network delays. Critical health decisions can't wait for WiFi.
Energy Efficiency through body-heat harvesting and kinetic charging means devices that never need plugging in. Flexible batteries conform to skin, making wearables you forget you're wearing. The always-on future requires power solutions that match biological persistence.
Integration With the Healthcare Ecosystem
Wearable data without clinical integration is just expensive self-monitoring. The real value emerges when continuous streams flow seamlessly into healthcare systems where providers can act on them.
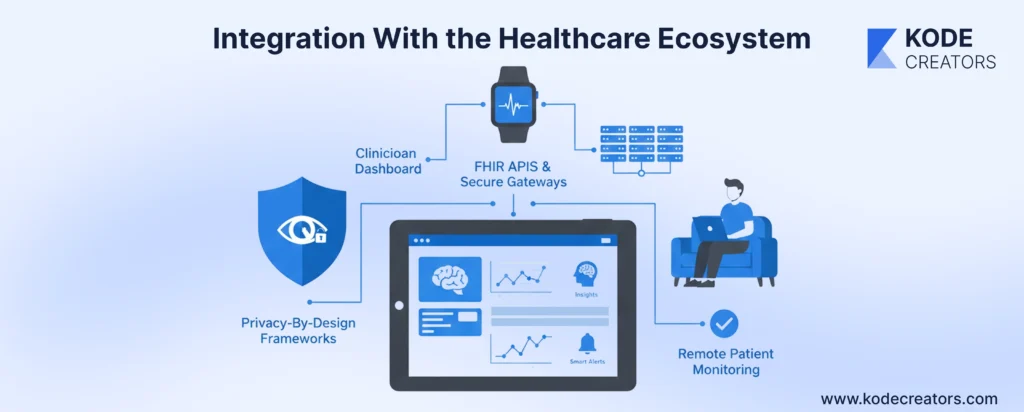
Data Flow Architecture
The pathway from wrist to medical record requires sophisticated translation. FHIR APIs convert consumer device data into clinical standards that EHRs understand – heart rate becomes structured observations, activity translates to functional assessments. Secure gateways aggregate multiple device streams before transmission, preventing the chaos of every fitness band trying to talk directly to hospital servers. Critical patients get real-time streaming while routine monitoring uses efficient batch updates.
Clinician Dashboards
Doctors don't have time to review 100,000 daily heartbeats. AI-powered dashboards filter noise, surfacing only significant changes:
- Baseline deviations that suggest problems brewing
- Trend visualizations replacing overwhelming data dumps
- Smart alerts that learn individual patterns to prevent alarm fatigue
- Drill-down capability when investigation is warranted
Remote Patient Monitoring Integration
RPM programs fail when they create parallel workflows. Successful integration means wearable data automatically triggers care protocols – recovery metrics adjust follow-up schedules, physiological responses confirm medication effectiveness, and 30-day trends enhance virtual visits. Billing systems capture appropriate reimbursement codes without manual intervention.
Privacy-By-Design Frameworks
Security starts at data creation, not transmission. Patients control granular sharing – cardiologists see heart data while employers get aggregated wellness metrics. Device-level encryption protects data before it leaves your wrist. Audit trails track every access, and zero-knowledge architectures ensure providers see insights without accessing raw personal data unnecessarily.
Benefits for Stakeholders
Patients finally own their health data and understand what it means. Continuous monitoring replaces anxiety-inducing annual checkups with daily reassurance. Personalized insights beat generic health advice – your wearable knows your patterns, not population statistics. Care becomes proactive, catching problems while they're fixable, not after they're expensive emergencies.

Physicians make decisions with complete pictures, not snapshots. Months of heart rhythm data reveals patterns invisible in office visits. Preventive alerts let doctors intervene before crisis calls. Documentation happens automatically – wearables capture objective data that supports clinical decisions and reduces liability.
Healthcare Providers see measurable improvements in metrics that matter. Readmission rates drop when post-discharge monitoring catches complications early. Emergency visits decrease as problems get identified at home. Operational costs fall while patient satisfaction scores rise – the combination executives dream about.
Insurers and Employers quantify wellness program effectiveness with actual data. Premium calculations reflect real risk, not demographic guesses. Workplace wellness initiatives show ROI through reduced sick days and lower claims. Preventive interventions cost pennies compared to treating chronic conditions that wearables help avoid. The data proves what works, eliminating expensive programs that only sound good.
Challenges Holding the Future Back
Data Security and Regulatory Bottlenecks create massive delays. FDA approval for medical-grade features takes years while hackers target health data worth 10x more than credit cards on black markets. Solution: sandbox regulatory environments and military-grade encryption from device to cloud.
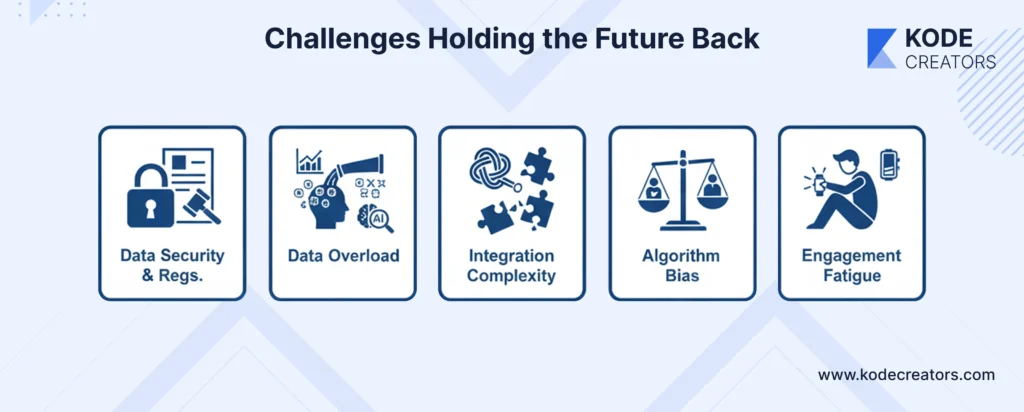
Data Overload drowns clinicians who already spend half their time on computers. Adding wearable streams without smart filtering creates noise, not insights. Fix: AI-powered dashboards that surface only actionable anomalies, not every heartbeat.
Integration Complexity makes hospitals want to scream. Every wearable speaks different languages, uses proprietary formats, requires separate platforms. Answer: industry-wide adoption of FHIR standards and vendor-neutral archives that translate between systems.
Algorithm Bias perpetuates healthcare disparities. Models trained on young, white, male athletes fail for elderly minority women. Resolution: diverse training datasets and continuous bias auditing across demographics.
Engagement Fatigue kills most wearable programs within six months. Initial excitement fades when people realize health improvement requires sustained effort. Strategy: gamification that evolves, social features that maintain accountability, and passive monitoring that doesn't require constant user interaction. The technology must become invisible while remaining valuable – background protection rather than foreground obligation.
The Future: Predictive, Adaptive, and Invisible Wearables (2025-2030)
Predictive Healthcare stops waiting for problems to appear. AI models analyzing years of wearable data forecast heart attacks months out, depression episodes weeks early, and infections days before fever. Your watch won't just track health – it'll predict your future health trajectory with uncomfortable accuracy.
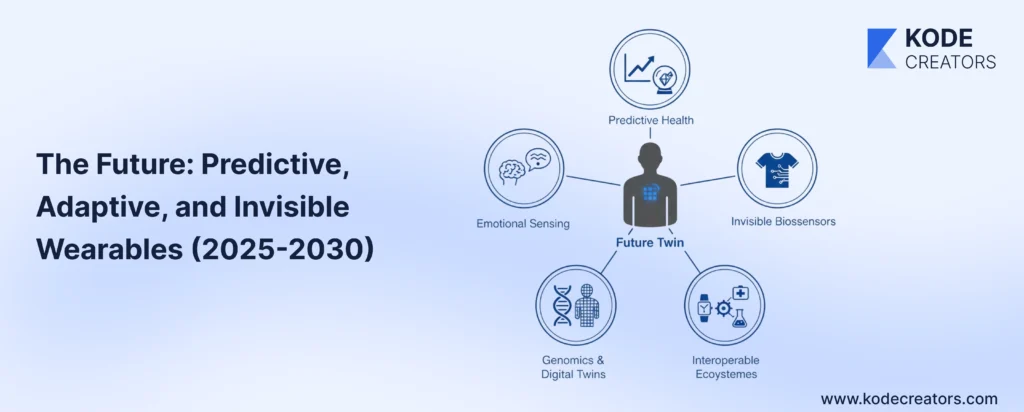
Biosensing Clothes and Implants make dedicated devices obsolete. Smart fabrics in regular clothing monitor everything current wearables do, invisibly. Temporary tattoos track glucose, implantable chips monitor cancer recurrence, contact lenses measure intraocular pressure. Health monitoring becomes ambient, not active.
Neural and Emotional Sensing brings mental health into continuous monitoring. Stress hormones in sweat, voice pattern changes suggesting depression, micro-expressions indicating anxiety – wearables will quantify emotional health like they currently track physical metrics. Preventive mental healthcare becomes possible when you catch problems before crisis.
Genomics Meets Digital Twins creates unprecedented personalization. Your genetic profile combined with years of wearable data builds a virtual you that tests treatments before you take them. Medications get optimized in simulation, not through trial and error on your body.
Interoperable Ecosystems finally connect everything. One dashboard shows wearable metrics, clinical records, genomic data, environmental factors – the complete health picture that's currently scattered across incompatible systems.
Conclusion:
Wearables have already saved thousands of lives by catching heart conditions people didn't know they had. But that's just the beginning. The next five years will transform these devices from health trackers into prediction engines that spot problems before biology does. The technology barriers have fallen – sensors are accurate enough, batteries last long enough, AI is smart enough. What remains is integration: getting healthcare systems to accept continuous data as seriously as annual physicals, training algorithms on diverse populations instead of Silicon Valley employees, and building privacy frameworks that protect without restricting innovation. T
he organizations that master this integration won't just monitor health – they'll guarantee it. Insurance companies will shift from treating disease to preventing it because wearables make risk visible and manageable. Hospitals will empty emergency rooms of preventable crises because problems get caught at home. The future of healthcare is in making treatment unnecessary. Wearables are the infrastructure of that future, turning every heartbeat into prevention, every breath into data, every step into a health decision. The only question is how quickly healthcare systems will embrace what patients already wear on their wrists.