Ever missed a doctor's appointment because it was too far? Or had to take a half-day off work just to wait in a room for a quick follow-up? It's annoying, isn't it? Patients shouldn't feel like getting care is a hassle. And doctors? They're trying to manage full schedules, long days, and patients who can't always show up.
Both doctors and patients can benefit from telemedicine's changes. More people are picking virtual visits now. In fact, 30% of U.S. patients now like virtual care for routine check-ups (and this number keeps growing). Telemedicine offers convenience, saves time, and allows millions to access care for those in rural areas or with mobility issues.
So what exactly is telemedicine, and how does it work? All you need to know about building a telemedicine platform is in this blog. Let’s get started.
1. What is a Telemedicine Platform and Why You Should Build It
A telemedicine platform is basically a clinic going digital. Patients can video chat with doctors, book appointments, get prescriptions, and access their medical records all from their phone or computer. No more waiting rooms, no more driving across town for a 10-minute check-up.
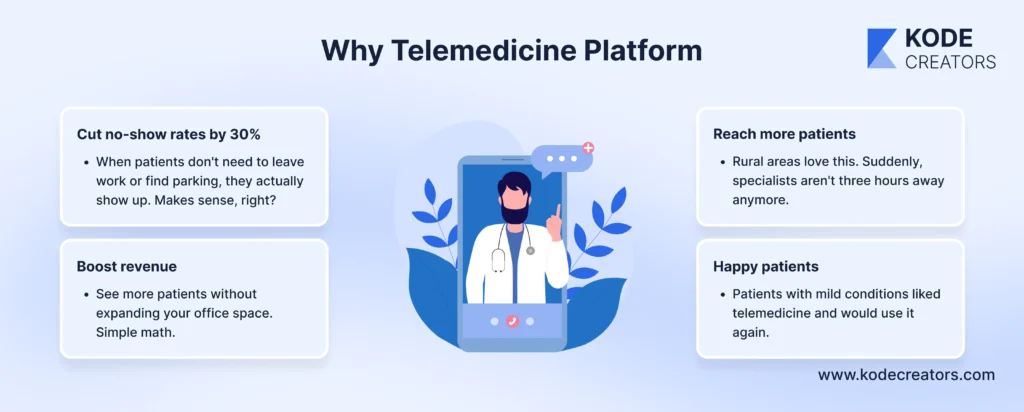
Here's why healthcare providers are jumping on this:
Cut no-show rates by 30% - When patients don't need to leave work or find parking, they actually show up. Makes sense, right?
Reach more patients - Rural areas love this. Suddenly, specialists aren't three hours away anymore.
Boost revenue - See more patients without expanding your office space. Simple math.
Happy patients - Patients with relatively mild conditions who tried telemedicine said they'd use it again. Convenience wins every time.
McKinsey found that telehealth is now 38 times more popular than before COVID. It's not going anywhere.
Who needs this? Solo doctors wanting to grow without overhead. Multi-specialty clinics coordinating care. Health systems competing with digital startups. Pretty much anyone is tired of playing phone tag with patients.
See, telemedicine isn't the future anymore - it's today. The question is whether you're building it or watching competitors do it first.
2. Core Features of a Modern Telemedicine Platform (Must-Have vs. Nice-to-Have)
Now comes the tricky part. Figuring out what features to include without turning it into a bloated mess that takes forever to build and costs a fortune.
Not all features are created equal. Some are absolute dealbreakers (skip these and you might as well not build anything). Others are nice extras that make you stand out. Let's break it down so you know exactly what to prioritize.

Must-Have Features (Non-Negotiable)
HIPAA-Compliant Video/Audio Calling
This is your bread and butter. Without secure video calls, you don't have telemedicine. We're talking end-to-end encryption here - not some basic Zoom call. Patient data needs military-grade protection, or you're looking at fines that'll make your head spin.
Secure Patient Authentication
You need to know patients are who the patients are. Two-factor authentication (2FA) is the minimum. Add biometrics if you can—fingerprint or face ID. One data breach from weak passwords and your reputation is toast.
Appointment Scheduling & Calendar Sync
Patients book online, it syncs with your Google Calendar or Outlook, and everyone's happy. No double-booking, no confusion. This feature alone cuts admin work by 40%.
In-App Messaging with Audit Trails
Quick questions shouldn't need a full appointment. But every message needs tracking for compliance. Think of it as texting with a paper trail—legally required, actually useful.
EHR Integration
Your telemedicine platform needs to talk to your existing systems. FHIR APIs or HL7 standards make this happen. Without it, you're manually copying notes between systems like it's 1995.
Digital Consent Forms
Privacy agreements, treatment consent, data sharing—all digital, all trackable. Patients sign once, you're covered legally. Doctors don’t need more scanning paper forms anymore.
Differentiators (The Competitive Edge Stuff)
AI-Powered Symptom Checker
Before the visit even starts, AI helps triage patients. Saves doctors 5-10 minutes per appointment by gathering info upfront. Patients feel heard, and doctors work smarter.
Automated Appointment Reminders
SMS and email reminders cut no-shows by another 20%. Set it and forget it. Your staff stops making reminder calls, and patients stop forgetting appointments.
Smart Intake Forms
Forms that adapt based on answers. Chest pain? The form asks about family history. Skin rash? It requests photos. Cuts intake time in half.
Real-Time Language Translation
Serving diverse communities? Built-in translation breaks down language barriers instantly. No interpreter scheduling, no delays.
Provider Dashboard with Analytics
See average visit duration, patient retention rates, and peak booking times. Data drives better decisions. You'll spot problems before they hurt your practice.
Pro Tip: Use the MoSCoW Method
Can't build everything at once? Use this framework:
Must have: Launch dies without it
Should have: Important but not day-one critical
Could have: Nice if the budget allows
Start with must-haves, get to market fast, then iterate based on actual user feedback. That's how you build something people actually use
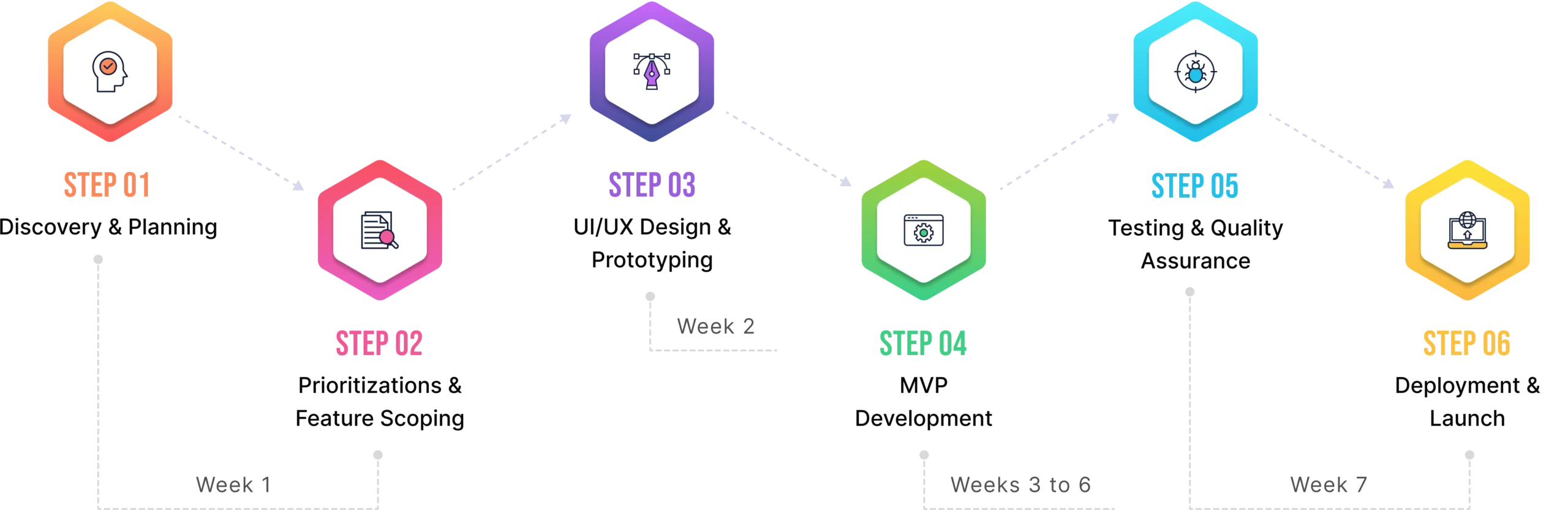
3. The Development Timeline (Phased Approach with Milestones)
Building a telemedicine platform isn't like throwing together a basic website. You're dealing with healthcare data, compliance rules, and actual patient care. Rush it, and you'll pay for it later. Take too long, and competitors beat you to market.
The realistic timeline that actually works is broken into bite-sized phases below, so you know exactly what happens when.

Phase 1: Discovery & Planning (2-4 weeks)
This is where you figure out what you're actually building. Sounds obvious, but if you skip this by any chance, don’t be surprised later about why your platform flopped.
You'll map out user personas (who's using this—tech-savvy millennials or seniors who barely email?). You need to create workflow maps showing how patients book, join calls, and get prescriptions. Sketch wireframes so everyone agrees on the layout before coding starts. Most importantly, build that compliance checklist—every HIPAA requirement, state regulation, and security standard you need to hit.
Skip this phase and you'll rebuild everything three months later.
Phase 2: MVP Development (3-5 months)
Time to build the core platform. Not every bell and whistle—just the essentials that make it actually work.
Video calls that don't drop every five minutes. A scheduling system that syncs with calendars. Build one secure login system that keeps hackers out. Basic EHR integration so you're not copying notes manually. This is your minimum viable product, so emphasis on "viable."
Three months if you're using existing frameworks. Five if you're building custom. Don't let anyone tell you they can do it in six weeks—they're either lying or cutting corners you can't afford to cut.
Phase 3: Testing & Compliance Audit (4-6 weeks)
Here's where you make sure everything's bulletproof. Penetration testing to find security holes before hackers do. HIPAA validation to confirm you're meeting every requirement. Drafting Business Associate Agreements (BAAs) with any third-party services you're using.
This phase feels slow because you're not building new features. But it's the difference between launching confidently and getting sued six months later. One data breach costs an average of $10.93 million in healthcare. Suddenly, six weeks of testing seems reasonable.
Phase 4: Launch - Soft Rollout (1-2 weeks)
Don't go live with the big demo of 500 users on day 1. Start small with onboarding 5 to 10 clinicians who'll give honest feedback. They'll find bugs your testing missed. UI issues that seemed fine to developers but confuse actual doctors as well as patients. Workflow problems you never anticipated.
Fix these issues while the user base is small. Much easier than dealing with angry emails from hundreds of providers.
Phase 5: Full Launch & Scaling (Ongoing)
Now you're live and growing. Add those could-have features that set you apart. Expand to new states (each has different regulations—fun times). Integrate with billing systems so payments flow automatically.
This phase never really ends. Healthcare tech evolves constantly. New regulations pop up. Competitors launch features you need to match. Plan on continuous updates and improvements.
4. Common Challenges & How to Avoid Them
Let's be real—building a telemedicine platform isn't all smooth sailing. You'll hit roadblocks that make you question why you started this in the first place. The good news? These problems are predictable. We've seen them happen dozens of times, and we know exactly how to dodge them.

Here are the four biggest headaches you'll face and how to avoid pulling your hair out.
Challenge 1: Poor Clinician Adoption
You built this amazing platform. Launch day arrives. And... doctors barely touch it. They stick to their old ways, complaining the new system is "too complicated" or "doesn't fit their workflow."
Sound familiar? It happens to 60% of healthcare tech launches.
The Solution: Get doctors involved from day one. Not just asking their opinion—actually co-designing with them during the MVP phase. Have them click through prototypes. Watch them struggle with confusing features. Fix those issues before you code.
Then, when you launch, run training webinars. Not boring PowerPoints—actual hands-on sessions where doctors practice with fake patients. Record these sessions so new staff can watch later. One practice we worked with saw adoption jump from 30% to 85% just by adding weekly 15-minute training sessions.
Challenge 2: Data Silos with EHRs
Your telemedicine platform works great. Your EHR works great. But they don't talk to each other. Now, staff are copying patient notes manually, wasting hours and making mistakes. It's like having two phones that can't call each other.
The Solution: Use FHIR standards from the start. It's the universal language that lets health systems communicate. Don't try to figure this out yourself—hire integrators who've actually worked with Epic, Cerner, or whatever system you're using.
Yes, experienced integrators cost more upfront. But they'll save you months of headaches and failed connection attempts.
Challenge 3: Low Patient Engagement
Patients sign up excitedly. Use it once. Then ghost you. Your platform becomes a digital ghost town with tumbleweeds rolling through empty appointment slots.
The Solution: Make it incredibly easy to use, at least for senior citizens and elders. Keep them well informed before and after the appointment, and send reminders. Send SMS reminders (not just emails that get buried). "Your appointment with Dr. Smith is tomorrow at 2 PM. Click here to join." Simple, direct, effective.
Gamify the onboarding process for millennials and teenagers. Build an interface that shows progress bars, achievement badges for cleared diagnoses, and rewards for showing up. It may sound silly, but it works.
Challenge 4: Regulatory Missteps
Nothing kills a telemedicine platform faster than compliance failures. One HIPAA violation, one missed state regulation, and you're looking at fines that'll make your CFO cry.
The Solution: Hire a HIPAA consultant before you write a single line of code. Not after. Not "when we have a budget." Now. They'll spot issues you never knew existed.
Document everything obsessively. Every security measure, every data access, every patient consent. When auditors come knocking (and they will), you'll hand them a beautiful binder of compliance proof instead of scrambling to explain yourself.
The platforms that succeed aren't the ones that avoid all problems—they're the ones that see them coming and prepare accordingly.
Conclusion:
Building a telemedicine platform isn't a weekend project. It's complex, sure—dealing with compliance, integration headaches, and getting both doctors and patients to actually use it. But it's completely doable when you have the right roadmap and an IT partner well-versed with HIPAA compliance and other regulatory needs for building a healthcare platform. Get started with the must-haves, test with a small group, then scale based on real feedback.
Whether you're a solo practitioner tired of no-shows or a health system competing with digital-first startups, the time to build is now. The question isn't if you should create a telemedicine platform - it's how fast you can get one up and running without compromising on what matters: security, usability, and actual patient outcomes.