Every morning, medical practices face the same inefficiency: patients completing paper forms while staff manually transcribe them into EHRs. The numbers are sobering as an average practice burns 15 hours weekly on patient intake data entry. That's nearly two full working days devoted to a task that technology solved years ago. Healthcare organizations are still paying $40,000+ salaries for human data entry even when the technology to eliminate this exists.
The solution to this? Implement true end-to-end automation where patient-entered data flows directly into your EHR without manual intervention. Modern intake automation validates insurance eligibility in real-time, checks for medication interactions as they're entered, and populates the exact right fields in your EHR while the patient is still in the waiting room. Practices using these systems report a 75% reduction in intake processing time and a near-elimination of data entry errors. The technology is proven, HIPAA-compliant, and is being deployed successfully across healthcare organizations of every size. The gap between practices still using clipboards and those with automated intake is widening rapidly, and it's measured not just in efficiency, but in patient satisfaction, staff retention, and competitive advantage.
Understanding the Modern Patient Intake Process
Patient intake encompasses everything that happens before clinical care begins: collecting demographics, insurance information, medical histories, current medications, allergies, consent forms, and payment details. It's the foundational data that drives every subsequent healthcare interaction, yet most practices still treat it as an administrative burden rather than a critical clinical process.
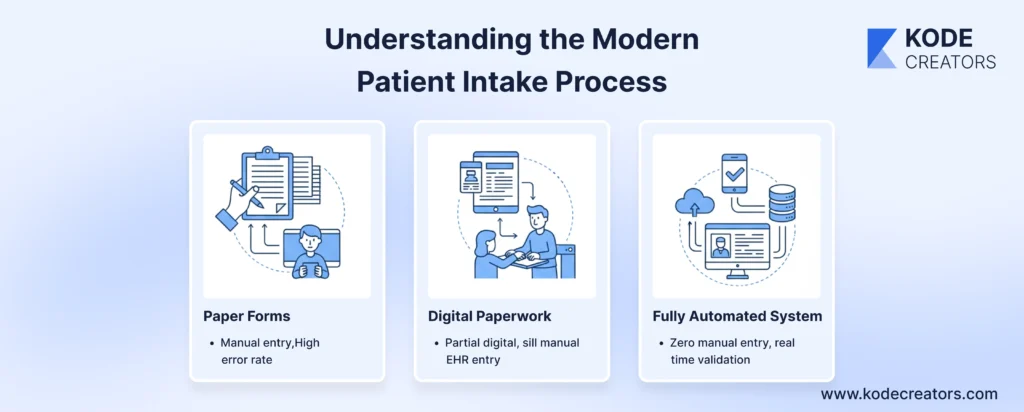
The evolution of intake reveals how far behind healthcare remains. Paper forms require patients to write information, staff to read it, and someone to type it into the EHR – three opportunities for errors. Digital forms on tablets eliminate handwriting issues but still require manual EHR entry. Staff still spend hours copying data from one screen to another, defeating the purpose of digitization. These partial solutions create what IT professionals call "digital paperwork" – electronic processes that replicate paper inefficiencies.
Fully automated systems represent the real transformation. Patient-entered data validates in real-time, maps to standardized medical codes, and flows directly into EHR fields without human touch. Insurance eligibility verifies instantly. Medication lists check against interaction databases. Consent forms route to appropriate folders. The core goal – zero manual entry from patient to EHR – isn't aspirational anymore. It's operational reality in forward-thinking practices where intake happens in minutes, not hours, and staff focus on patient care instead of data entry.
Key Components of an Automated Patient Intake System
Digital Front-End: Where Patients Actually Want to Engage
The front-end is where automation succeeds or fails. Modern systems offer multiple entry points: mobile-responsive web forms patients complete at home, tablet applications for waiting rooms, or self-service kiosks for walk-ins. The best platforms adapt to user needs – large fonts for elderly patients, multiple language support, smart branching that skips irrelevant questions. If a patient indicates no surgical history, they don't see 20 questions about previous procedures. Mobile optimization is critical; 67% of patients prefer completing forms on their phones before appointments. Progressive save features ensure partial completions aren't lost, and returning patients see pre-populated fields they can verify rather than re-enter.
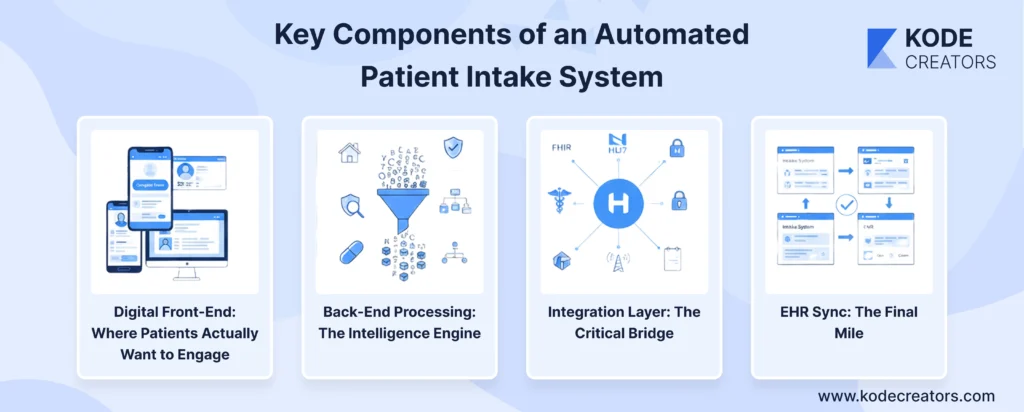
Back-End Processing: The Intelligence Engine
Raw patient input is messy. The back-end processing layer transforms chaos into structured data. Address validation ensures "123 Main St" becomes properly formatted entries with ZIP+4 codes. Insurance verification runs eligibility checks against payer databases in real-time, flagging coverage issues before the appointment. Medication reconciliation matches patient-entered drug names against RxNorm databases, catching potential interactions. Data mapping converts free-text entries into standardized codes – "high blood pressure" becomes ICD-10 code I10. This layer also handles business rules: flagging incomplete fields, requiring additional information for specific conditions, and routing special cases for manual review.
Integration Layer: The Critical Bridge
The integration layer determines whether automation actually works or just creates new data silos. Modern systems use FHIR APIs for real-time data exchange with EHRs, though many still require HL7 interfaces for legacy systems. Middleware platforms handle protocol translation, ensuring data formatted for one system translates correctly to another. Encryption happens here – TLS 1.3 for transmission, AES-256 for temporary storage. API management includes rate limiting, retry logic for failed connections, and queuing for systems that can't handle real-time updates. Smart platforms maintain audit logs of every transaction, crucial for troubleshooting and compliance.
EHR Sync: The Final Mile
EHR synchronization is where many solutions fail. True automation requires bidirectional sync – not just pushing data to the EHR, but pulling updates back to keep intake forms current. Field mapping must be precise; "emergency contact" in the intake form must populate the exact corresponding field in Epic, Cerner, or whatever EHR you're running. Modern systems handle partial updates, conflict resolution, and maintain data integrity across systems. Real-time sync means staff see updated information immediately, while asynchronous options handle high-volume scenarios without system overload.
Step-by-Step Workflow: From Digital Form to EHR
Step 1: Patient Engagement
The workflow begins when patients receive a secure link via text or email 48 hours before their appointment. They complete forms on their device of choice – phone, tablet, or computer. In-clinic patients use waiting room tablets or kiosks. Smart forms guide patients through relevant questions only; diabetics see glucose monitoring questions while others skip them entirely. Auto-save prevents lost work, and patients can pause and resume anytime.
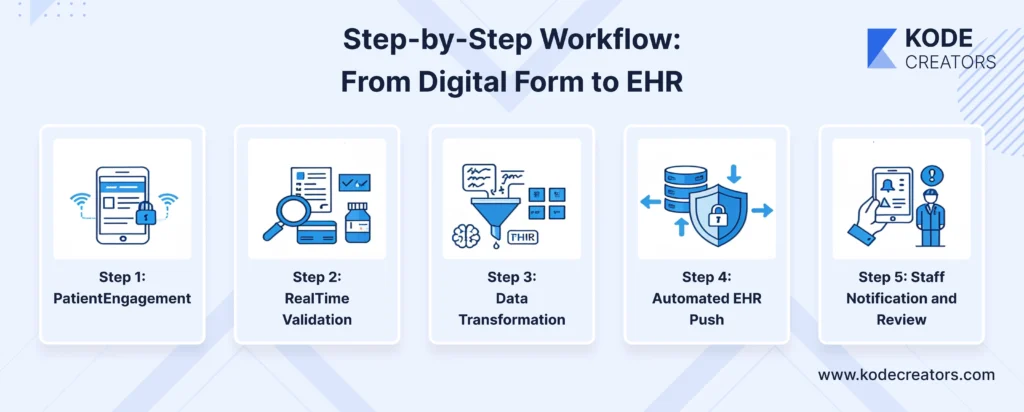
Step 2: Real-Time Validation
As patients enter information, the system validates everything immediately. Addresses verify against USPS databases. Insurance IDs check against payer systems, confirming coverage and copay amounts. Medication names auto-complete from RxNorm databases, preventing spelling errors that cause dangerous misidentifications. Invalid entries trigger helpful prompts – "Insurance ID should be 9 digits" – not generic error messages.
Step 3: Data Transformation
Validated data converts into standardized medical formats. Patient-friendly terms become clinical codes: "heart pills" maps to the specific beta-blocker in their history. Free-text symptoms transform into structured FHIR Observation resources. The system maintains both patient-entered originals and clinical translations for accuracy verification.
Step 4: Automated EHR Push
Structured data flows directly into the EHR through secure APIs – no human intervention required. Each field maps precisely: allergies populate the allergy module, medications update the current med list, insurance information fills billing fields. The push happens in seconds, not hours.
Step 5: Staff Notification and Review
Staff receive dashboard alerts when intake completes. They see flagged items requiring attention – expired insurance, concerning symptoms, medication conflicts. Everything else is already in the EHR, ready for the visit.
The Two-Way Advantage
Here's what separates good systems from great ones: bidirectional synchronization. When providers update medications during visits, those changes reflect in future intake forms. Patients see their current information, not outdated data from six months ago. They verify and update rather than re-enter, reducing intake time by 60% for returning patients while maintaining accuracy.
Benefits of Full Patient Intake Automation
Operational: Reclaiming Lost Hours
Full automation delivers 70-80% reduction in administrative time spent on intake. Staff who previously spent entire mornings entering forms now handle complex patient needs instead. Data entry errors – the source of countless downstream problems – virtually disappear. Automated systems achieve 99%+ accuracy compared to 92% for manual entry. That 7% difference represents thousands of corrected claims, prevented medication errors, and avoided patient frustrations. Practices report freeing up 15-20 hours weekly, equivalent to adding half a full-time employee without the salary.
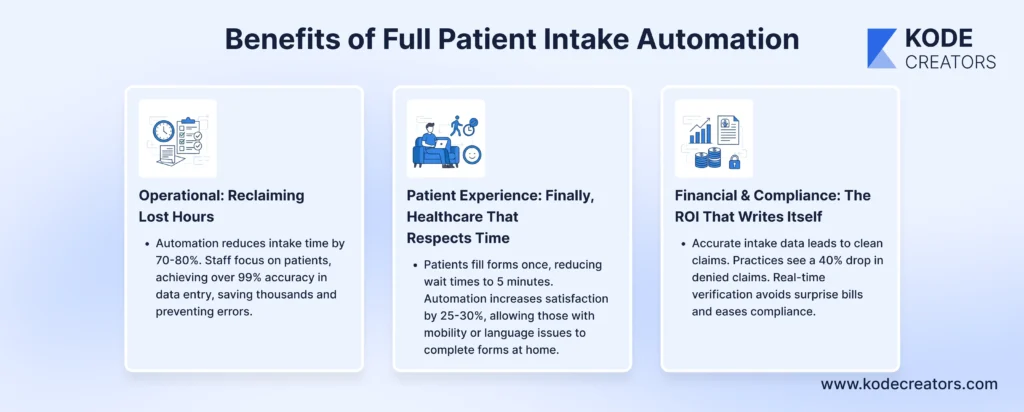
Patient Experience: Finally, Healthcare That Respects Time
Patients complete forms once, not repeatedly. Wait times drop from 20 minutes to 5 when intake happens before arrival. The elimination of redundant questions and clipboard juggling transforms the arrival experience. Patient satisfaction scores increase 25-30% when practices implement full automation. More importantly, patients with mobility issues, visual impairments, or language barriers can complete forms at their pace, with appropriate accommodations, from home.
Financial & Compliance: The ROI That Writes Itself
Accurate intake data means clean claims. Practices see 40% reduction in denied claims due to demographic or insurance errors. Real-time insurance verification prevents surprise bills and payment delays. Every transaction creates automatic audit trails, simplifying compliance reporting and reducing audit preparation from weeks to hours. The average practice recovers implementation costs within four months through improved billing accuracy alone.
Compliance and Security Essentials (Non-Negotiable)
HIPAA compliance isn't optional for patient intake systems – it's the foundation. Every data transmission requires TLS 1.3 encryption, while stored data needs AES-256 encryption, including temporary cache files that developers often forget. Patient forms sitting in browser storage for auto-save functionality? Encrypted. PDFs generated for records? Encrypted. API payloads between systems? Encrypted. One unencrypted data point can trigger investigations that cost millions.

Access control extends beyond simple passwords. Role-based permissions ensure registration staff see demographics but not psychiatric notes. Multi-factor authentication is mandatory for any system access. Comprehensive audit logs track every view, edit, and export – not just for compliance, but for investigating discrepancies. These logs themselves require encryption and retention policies matching state requirements.
Business Associate Agreements aren't suggestions – they're legal requirements for every vendor touching patient data. That includes form builders, cloud hosts, API gateways, even analytics platforms. Missing one BAA makes you liable for their security failures. Secure cloud hosting means HIPAA-compliant infrastructure with SOC 2 certification, not just any AWS account. Regular penetration testing, vulnerability assessments, and disaster recovery plans transform from nice-to-haves into evidence of reasonable security measures. When auditors arrive, they want documentation proving security was built-in, not bolted on after deployment.
The Future: Intelligent Intake Beyond 2025
The next generation of intake systems won't just collect data – they'll anticipate needs. Predictive forms are already emerging that analyze historical patterns to pre-populate likely responses. A patient with quarterly diabetes check-ups sees pre-filled medication lists, recent glucose readings from connected devices, and relevant symptom questions based on their last visit. The system knows what changed since last time and asks only about those deltas.
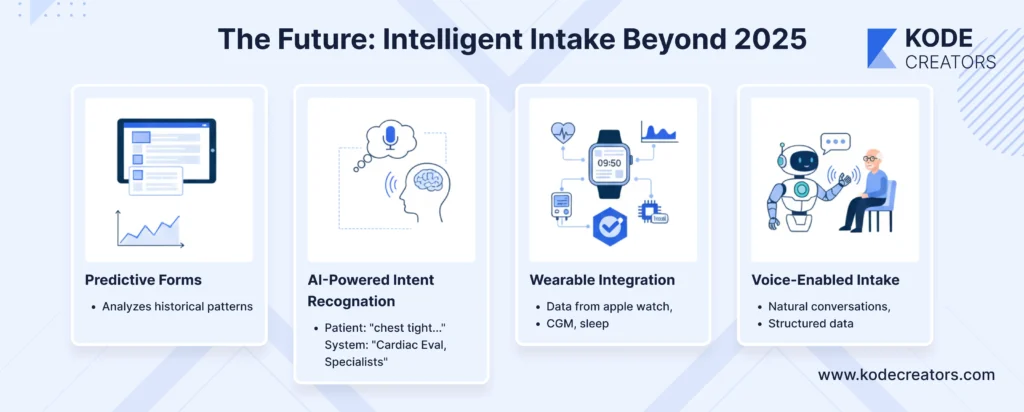
AI-powered intent recognition transforms how patients describe their needs. Instead of selecting from dropdown menus, patients write "chest feels tight when climbing stairs" and the system identifies probable cardiac evaluation needs, suggests relevant specialists, and prepares appropriate screening questions. Natural language processing eliminates the guesswork of matching symptoms to medical terminology.
Wearable integration is moving from novelty to necessity. Apple Watch heart rhythms, continuous glucose monitor trends, and sleep pattern data flow into intake systems before appointments, giving providers context that patient memory can't match. Telehealth pre-visits let AI chatbots conduct initial intake conversations, asking follow-up questions based on responses and flagging concerns for providers.
Voice-enabled intake serves aging populations and accessibility needs while reducing form fatigue. Patients have natural conversations with AI assistants that extract structured data from unstructured dialogue. By 2027, we'll see intake systems that know patients better than they know themselves, predicting problems before symptoms appear.
Final Thoughts
Patient intake automation isn't just another digital transformation initiative – it's the gateway to every other healthcare innovation you're planning. You can't deliver personalized care when you're drowning in data entry. You can't improve patient outcomes when staff spend hours transcribing forms instead of engaging with patients. The technology we've outlined isn't theoretical or emerging – it's operational in thousands of practices today, delivering measurable ROI within months. The divide between automated and manual intake processes is becoming a competitive canyon. Practices still using clipboards are losing staff to burnout, patients to frustration, and revenue to inefficiency. Meanwhile, automated practices are scaling without adding administrative overhead, improving patient satisfaction without adding wait time, and capturing clean data that drives better clinical decisions. The question isn't whether to automate patient intake – it's whether you'll lead this transformation or scramble to catch up when patients start choosing providers based on their digital experience.